Diabetes Decision Support
Using data to assist diabetes patients
Summary
In 2016, Dexcom was exploring ways to leverage continuous glucose monitor (CGM) and other contextual data to assist intensive insulin therapy (IIT) patients between clinic visits. The project goal was to identify opportunities for decision support features and benefits to users.
My Role
My startup Databetes was hired to conduct discovery research and provide a synthesis report. I conducted all the interviews. I managed 2 additional UX designers and a UX researcher who assisted on the project.
Background
CGM adoption among IIT patients has grown steadily in recent years. The technology has proven itself to be just as accurate as fingerstick measurements of blood glucose, yet infinitely more convenient. Patients who use CGM become to rely on new glucose readings every 5 minutes to help them make in the moment treatment decisions.
While the value of real time CGM data has become clear to the market, Dexcom was interested in finding additional ways to help patients through its data. The aim was to help patients improve health outcomes while also adding functionality that would increase brand loyalty.
Research
In 2016, Databetes began planning broad, primary research on IIT patients and healthcare providers. Topics included:
Daily Challenges: The everyday struggles patients face managing their glucose levels
Habits and Attitudes: How patients approach overnight glucose level management, meal bolusing, basal dosing, hypoglycemia treatment, hyperglycemia corrections, exercise & activity
Evolving Approaches to Self-Management: How patient thinking and behaviors have changed from diagnosis to current state
Clinical Instruction: How healthcare providers teach patients about self-management
Clinician Workflows: Processing of diabetes data to proposed treatment changes
I conducted a total of 74 interviews at three site locations around the United States.
50 Patients on IIT
29 Type-1 patients
21 Type-2 patients on IIT
24 Clinicians Treating IIT Patients
11 Endocrinologists
3 Primary care physicians
10 Certified diabetes educators, registered nurses and physician assistants
Patients were recruited for diversity in insulin delivery method, time since diagnosis. CGM usage, age, income, education level, and ethnicity.
Process
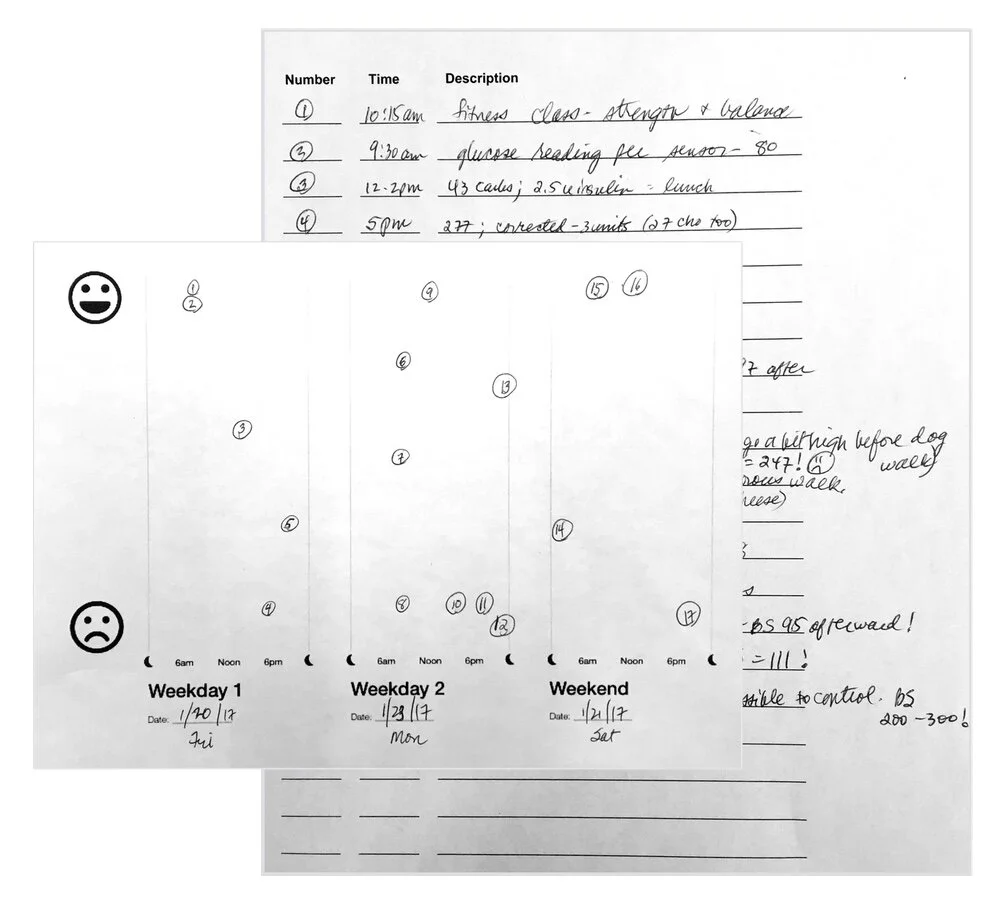
Patients were asked to do 3 days of self-tracking homework assignment. Interviews lasted 75 minutes.
Self-tracking homework from a patient.
Interviews with clinicians were 60 minutes with no required pre-work.
After completing the interviews, the team worked to synthesize the data.
Themes
A number of key idea were common throughout the interviews.
Mental Burden: Patients spoke frequently of a condition that was always on their mind, generating “a low hum of anxiety.”
“It’s always on your mind. It’s kind of like a mental jail. It’s like you can never be free of not thinking about it.
Type-2 patient on IIT, Atlanta, GA
“It’s all day, every day, it’s something you constantly have to be on top of. It’s never ending, it’s never ceasing, it’s relentless. I think about it more than I think about anything else.”
Type-1 patient, Atlanta, GA
“Whether you realize it or not, it’s a very serious disease that can turn on a dime, and it dominates… I’m not saying it dominates every second of your time. But in the background, it’s always dominating because it needs to be as close to perfect as possible if you want to see and have kidneys and not have pain.”
Type-1 patient, Houston, TX
Finding Balance: Patients are pulled in many directions, with their diabetes competing with work, family, and rest of their life. Clinicians noted a distinction between a patient’s ability to manage their diabetes relative to the time and effort they were willing to focus on it.
Food Choices: Patients with diabetes vary widely in their approach to meals. At one end of the spectrum, some patients continue diets of fast food and processed foods. Alternatively, some patients drastically scale down their carbohydrate intake to minimize their insulin dosing. For others, each day can be a struggle between what they want to eat and the knowledge of what it will do to their glucose.
Meal Dosing: Knowledge of carb counting and the basics of nutrition also vary considerably. Endocrinologists tend to make judgements on whether their patients can accurately calculate their carbs based on levels of engagement, age, and education level. Certified Diabetes Educators (CDEs) tend to be more flexible in their approach, reverting to fixed doses or sliding scales for patients who are unable to carb count.
Knowledge of Nutrition: Clinicians spoke of multiple challenges for patients, including struggling to estimate portions, lack of understanding of food labels, and guessing about meals eaten out.
“There’s a lot of misinformation out there. They’ve gotten misinformation from their physicians, their neighbors, their family members, and they’re bombarded with that, even after they come in and get education. They hear the wrong stuff, that they can’t eat sugar, that they shouldn’t eat carrots, they can’t eat anything white (that’s the biggie), that they need to be on a special ‘diabetic diet.’ So we try to dispel all those myths right out of the gate.”
Certified diabetes educator, Atlanta, GA
Behavior Change: Several patients had significant “wake up” events around their diabetes that motivated them to change their approach to self-management. For others, meeting a new clinician or fellow patient becomes a significant factor for improving their own care. Once motivated to change, nearly all patients spoke of simple trial and error as the only way to work through problems.
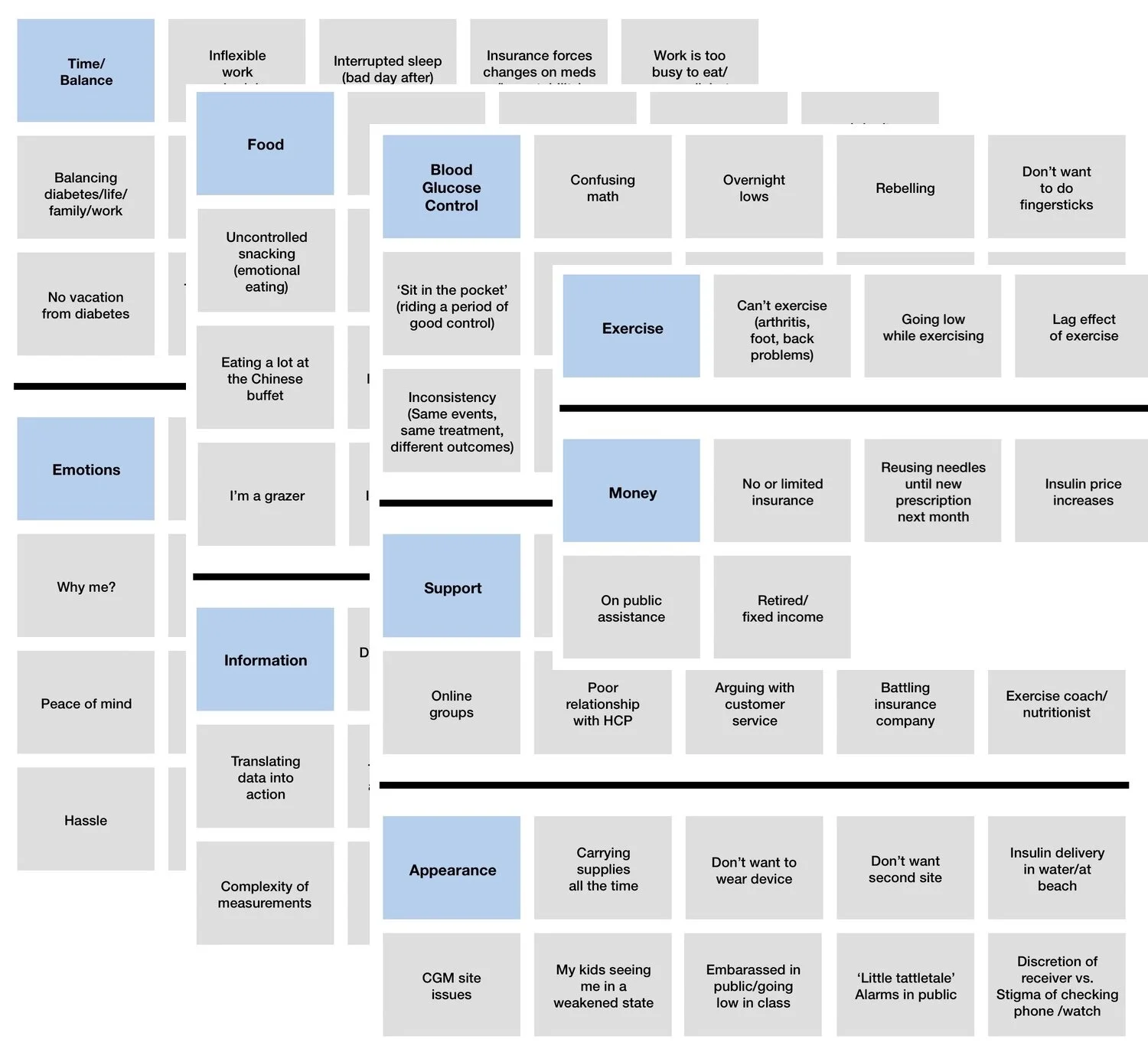
Grouping of pain points
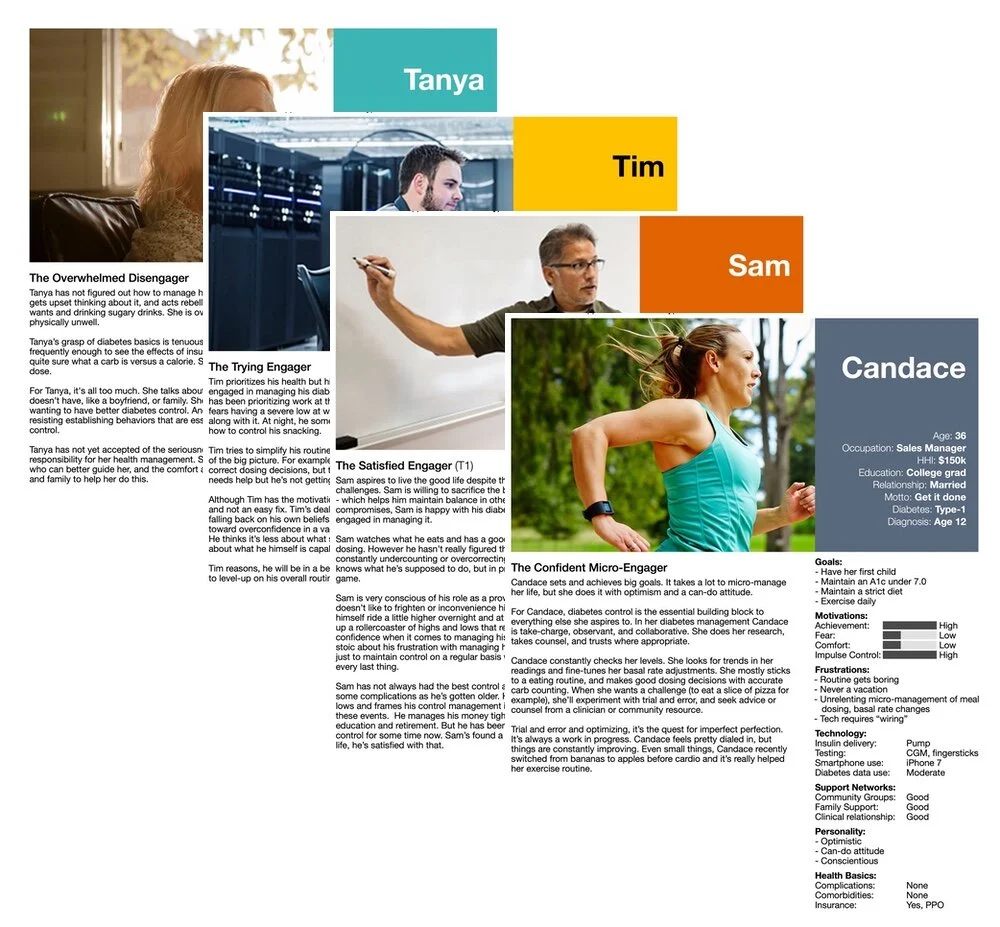
Patient Personas
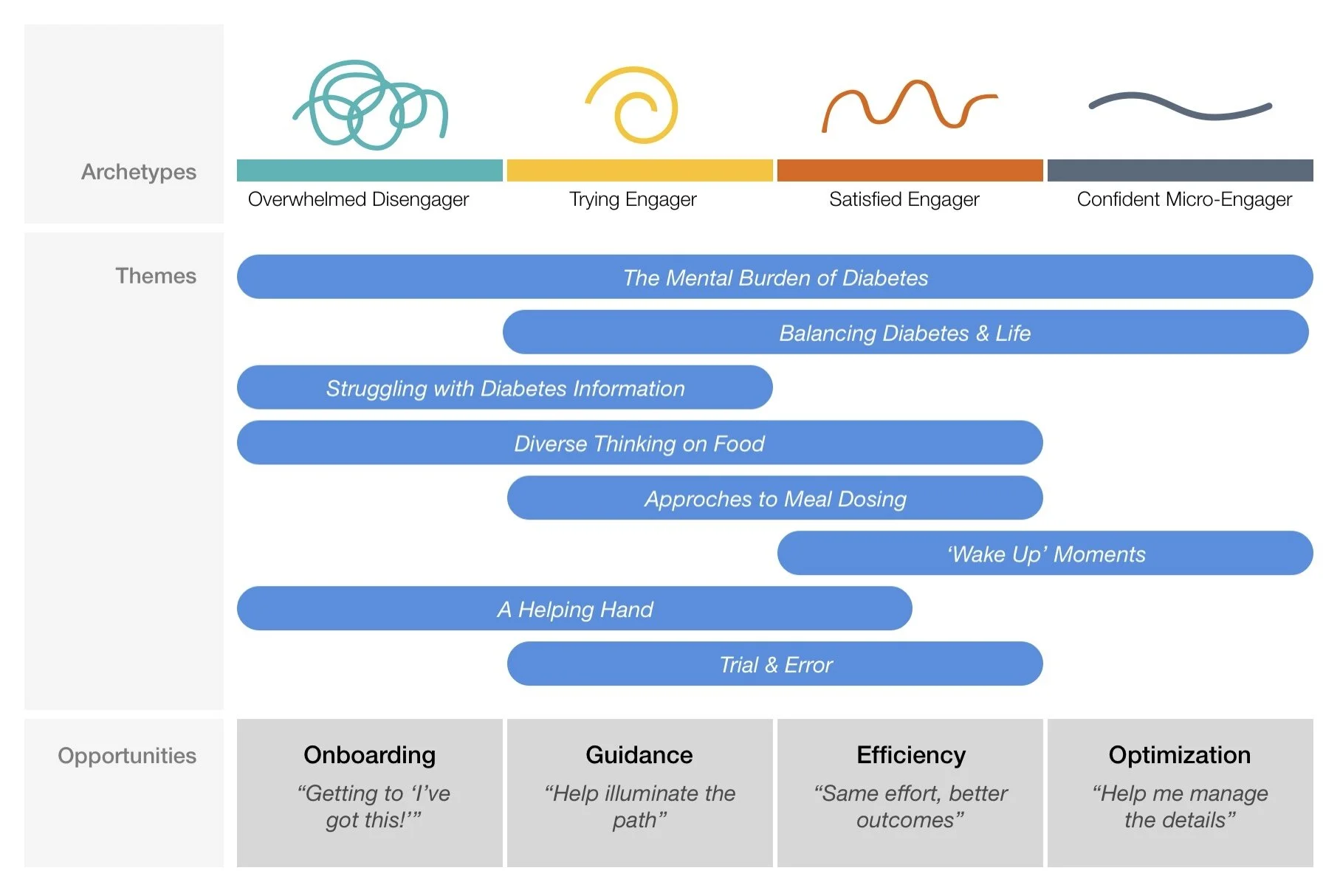
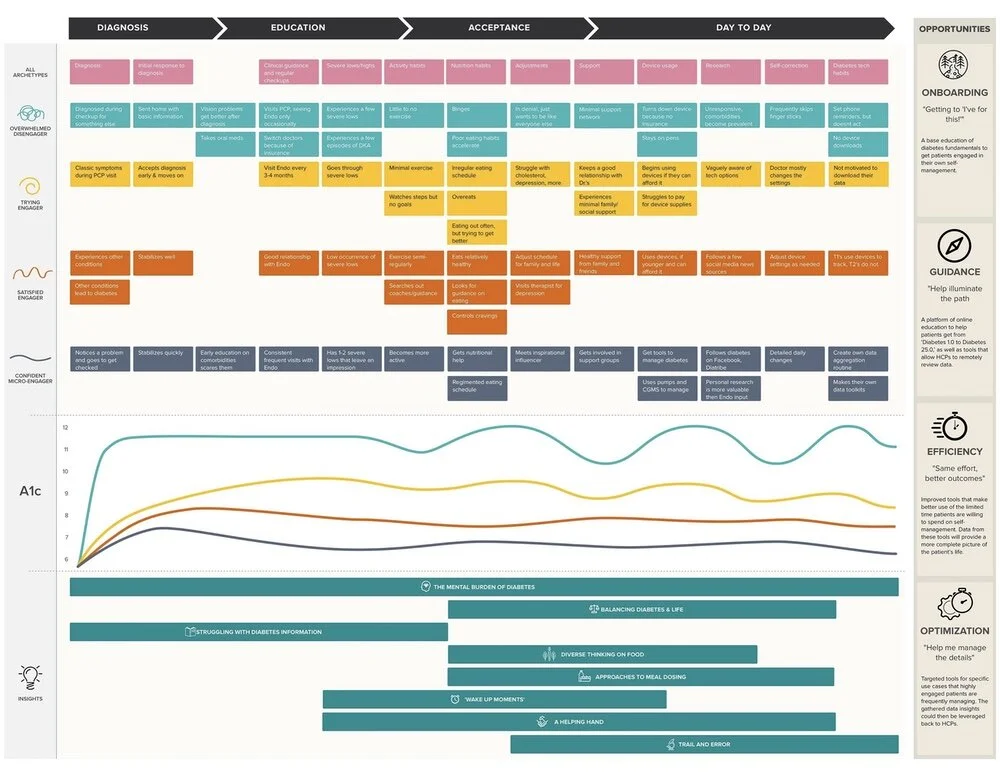
We generated 4 personas based on the user interviews and homework.
Overwhelmed Disengager: Individuals with poor A1c’s who are not making recent progress.
Trying Engager: Bear similarities to the ‘Confident’ and ‘Satisfied’ Engagers, but are differentiated by a characteristic serious blocker - a problem or issue that prevents them from achieving the control they desire.
Satisfied Engager: The largest group, they are engaged in their own care and have good A1c’s. A major differentiator is their interest in finding balance between the various commitments in their life to diabetes, work and family.
Confident Micro-Engager: Represents the top end of individuals in terms of time allocated to diabetes. They are highly engaged in their care, have the lowest A1c’s and make diabetes a high priority.
Opportunities
Based on the themes and personas, we identified the areas that showed the most promise for this patient population.
Onboarding: “Getting to ‘I’ve got this’”
Guidance: “Help illuminate the path”
Efficiency: “Same effort, better outcomes”
Optimization: “Help me manage the details”
We also produced journey maps for each of the personas, mapping them to the opportunities.
Closing Thoughts
Major research projects like this are memorable experiences. Medical device companies hear often from their most engaged customers who want additional “superuser” features. Getting into the field reminds us how a significant percentage of patients are doing the best they can to stay healthy while also managing the rest that life brings. The cost of healthcare, access to support networks, and a host of other variables have a profound impact on patient outcomes.
Clinician and researcher Dr. Joyce Lee of the University of Michigan blogs at Doctor as Designer. She highlighted the role that service design could play in guiding a patient to better outcomes.
“People come for clinic visits, but there isn’t growth. There isn’t a way to guide them along the process, to go from Diabetes 1.0 to Diabetes 25.0… The question is what is healthcare delivery’s role in guiding that progression of understanding, of learning new opportunities, of adopting new technologies.”
Devices like CGMs, insulin pumps, and connected insulin pens are powerful devices. As competition increases, these will likely become commodities, with declining prices translating to increased adoption. Yet patients will continue to struggle to make sense of all this information, glean the right insights, and translate it into a plan of action. Technology will be able to assist in this challenge too, either by generating workflow enhancements for busy healthcare providers or new ways to engage and guide patients in between clinic visits.
Diabetes remains an emotional disease. The mental burden of diabetes is the theme that all patients voiced, no matter their persona. A combination of personal support and technology continues to show the most promise for improving health outcomes and lowering the cost of care.