Food & Diabetes
Two approaches to a key challenge
Summary
Food is complicated. It’s personal, emotional, social, and potentially confusing. It affects everyone’s health, including people with type-1, type-2, or pre-diabetes. It’s also an outlier in the world of sensors, a challenge to accurately measure or auto-track in the background.
Research shows that patients need help managing their meals and glucose, one that aligns with their treatment goals, lifestyle, and overall approach to diabetes management.
My Role
I’ve worked on this topic in multiple ways. Documented here are two projects. The first is Meal Memory, a mobile app I created with my startup Databetes. I led the research, design, and marketing of the product.
Second is the Nutrition Data Strategy I produced for Dexcom. It informed the approach to several software products and the company’s Decision Support project.
Background
As someone living with diabetes for several decades, I’ve spent lots of time thinking about food and nutrition. I do this in relation to my glucose control, energy level, exercise regimen, weight, and interest in becoming a better cook. I’ve learned a lot, and still have plenty more to learn.
Food is also interesting to me as a designer. Goals, motivation, knowledge, and support systems vary greatly among patients with diabetes. There’s a range of problems to be solved and no simple solutions.
Project 1: Meal Memory
To begin tackling the challenge of managing food I started with what I know best, my own diabetes management. I set out to create a tool to help me better manage my own meals. I did this while experimenting with self-tracking.
ITP & Databetes
In 2011, I started grad school at NYU’s ITP (Interactive Telecommunications Program). This was a major pivot for me from my previous career as a photojournalist based in Beijing and New York. I was motivated by an interest in building better tools for patients like me. I’d long been impressed with the hardware available to diabetes patients, including my insulin pump and continuous glucose monitor (CGM). Yet the software continued to leave me underwhelmed. It failed to make good use of all my medical data, let alone other lifestyle data it could be collecting like food and exercise. The burden was still on me to gather all this information, process it, and make daily treatment decisions. There had to be a better way.
At the same time I worked to the startup I founded named Databetes off the ground. If the software I wanted didn’t exist, I wanted to help create it. I threw myself into learning product design and how to draft a business plan.
Design Challenge
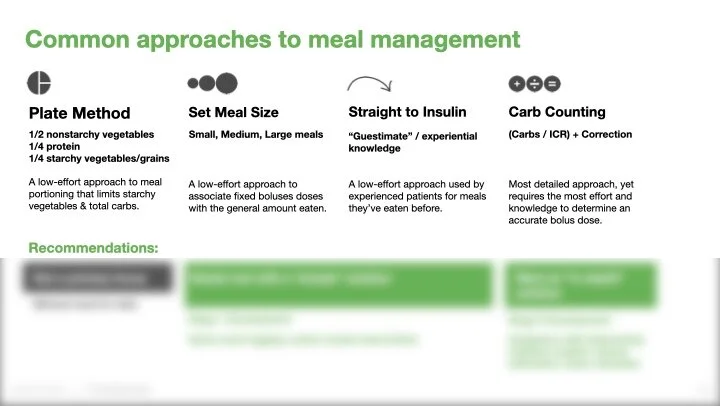
Having type-1 diabetes means I am an IIT (intensive insulin therapy) patient. I need both long-acting and mealtime insulin to survive. Narrowing the project scope to IIT patients like me meant focusing on carbs. One of the biggest challenges I face on a daily basis is how much insulin to take when I eat. Proteins, fats, and other types of nutritional content do affect my glucose, but in a minor way. The primary consideration when calculating a mealtime dose is the amount of carbohydrates. With that, you can calculate how much insulin is needed. IIT patients often know their insulin-to-carb ratio (mine is 1:10, 1u of fast-acting insulin to every 10 grams of carbs).
When I see food, I start counting carbs. Patients are taught guidelines on how to make this calculation, such as translating pieces of bread and the size of fruit into estimates in grams. We jokingly refer to these as “guestimates.” Only when eating food with a nutrition label can you be more sure of the carb total. There’s also estimates based on experience. One meal may seems similar to a 50g of carb meal I’d eaten recently.
You translate the carbs to insulin, check your current glucose, dose accordingly, check your glucose again a few hours later, then deliver a correction dose if needed (or have to treat a low glucose with sugar if you dosed too much). It’s an imperfect process.
The daily mental burden of diabetes comes from challenges like these, trying to recall and process all this information. In my head I had two kinds of meals: those I had “solved” for and those I hadn’t. I kept my breakfast the same because I’d learned exactly how much to dose for it that my glucose was in range afterwards. But those tricky meals to calculate the carb count of or the meals you ate only occasionally proved to be the biggest challenges. Was it 8 or 10 or 12 units I’d taken last time? That difference in dose size was enough to leave me tired and sluggish for hours afterwards if I got it wrong. A few days like that a week, over months and years adds up and puts you at greater risk for a long list of diabetes complications.
Discovery Research
I interviewed several dozen IIT patients and I learned that they also struggled with meal dosing. While agreeing that it was a problem, the vast majority of people I spoke with did not log any of their meals. Existing tools made self-tracking a cumbersome and time consuming process. Apps were mainly text-based and had multiple required fields. It was too much of a disruption when you had food in front of you, especially when eating with friends, to take a minute or two to enter information. The idea of doing it every meal seemed daunting (if you remembered). Plus, the reward for the work was minimal. The software often did not provide actionable feedback. Searching through past entries was also a chore. As a result, even the most motivated patients would give up after logging a few meals.
Additional Voices
As I explored this topic, I also researched healthcare providers, behavioral psychologists, and others active in the space. An early inspiration was Dr. Joyce Lee, a pediatric endocrinologist and researcher at the University of Michigan. Dr. Lee’s blog at doctorasdesigner.com highlighted her interest in the intersection of design and healthcare.
Credit: Dr. Joyce Lee, https://www.slideshare.net/joyclee/doctor-as-designer-26625644
One theme from her presentations is that we give patients bad tools and then wonder why they’re not successful. She focuses on the power of participatory design to empower and engage both patients.
I also learned about Stanford University behavioral scientist BJ Fogg. Two important points from his work resonated with me in regards to this project. First, his Behavioral Grid gave me a framework to think about influencing behavior. It takes time and effort to create a new habit. I also found value in his behavioral model focused on ability, motivation, and prompts. I liked the simplicity of focusing on making things easier to do as a way to get people to do them more often.
Definition
Research highlighted several important themes for me:
Opinions on Self-Tracking: Many patients had a visceral reaction to even the idea of logging meals. It was associated with something that was annoying, a waste of time, something to be done only if required by a doctor. This was interesting to me because apps like Instagram were becoming more popular at the time. They required a similar amount of time and effort to create an entry, yet produced infinitely more delight.
Scope of Engagement: A major challenge of managing chronic conditions is sustainability, creating and maintaining long-term healthy behaviors. But the idea of doing something forever is daunting. When it comes to meal logging, what is the right expectation? From my own experience, I’d already made a distinction between challenging and not challenging meals. I wanted to design an app that helped you, without expecting you to use it for every meal. In fact, if it helped you “solve” how to manage a challenging meal, usage of the app might actually go down.
Easy Input: Building on BG Fogg’s work, I wanted to lower the bar for logging a meal in terms of both time and effort. My thinking was that any information entered is already better than nothing (the current norm for most patients). Pulling on the Instagram thread, I focused on a photo-based solution. It was quick, easy, and a behavior that people were already doing. Other fields like text entry, a carb estimate, or an insulin dose should be optional. Taking a photo of food while eating with friends carried none of the social stigma that patients were self-conscious about when using other event entry apps.
Understanding Cause & Effect: The core question patients wanted answered was how did this meal affect my glucose? Presenting this information to users was essential. It required a pre-meal and a post-meal glucose reading. Gathering and presenting that data was the challenge.
Design for Repeated Meals: Once a patient has gone to the trouble of entering a meal, they also need to be able to find that entry again if needed. People are creatures of habit, frequent their favorite restaurants, and frequently order the same dishes. A past entry showing how a meal affected glucose is key knowledge. It is a much better starting point than starting at the beginning again with a new “guestimate” carb count. Once again, a photo-based system showed promise. It allowed for quick scanning of past entries. A photo can also generate an emotional reaction, jogging our memory of the social situation we were in when we ate the meal. With this system, the user gets closer with each entry to moving it from the challenging meal to the not challenging column.
Design
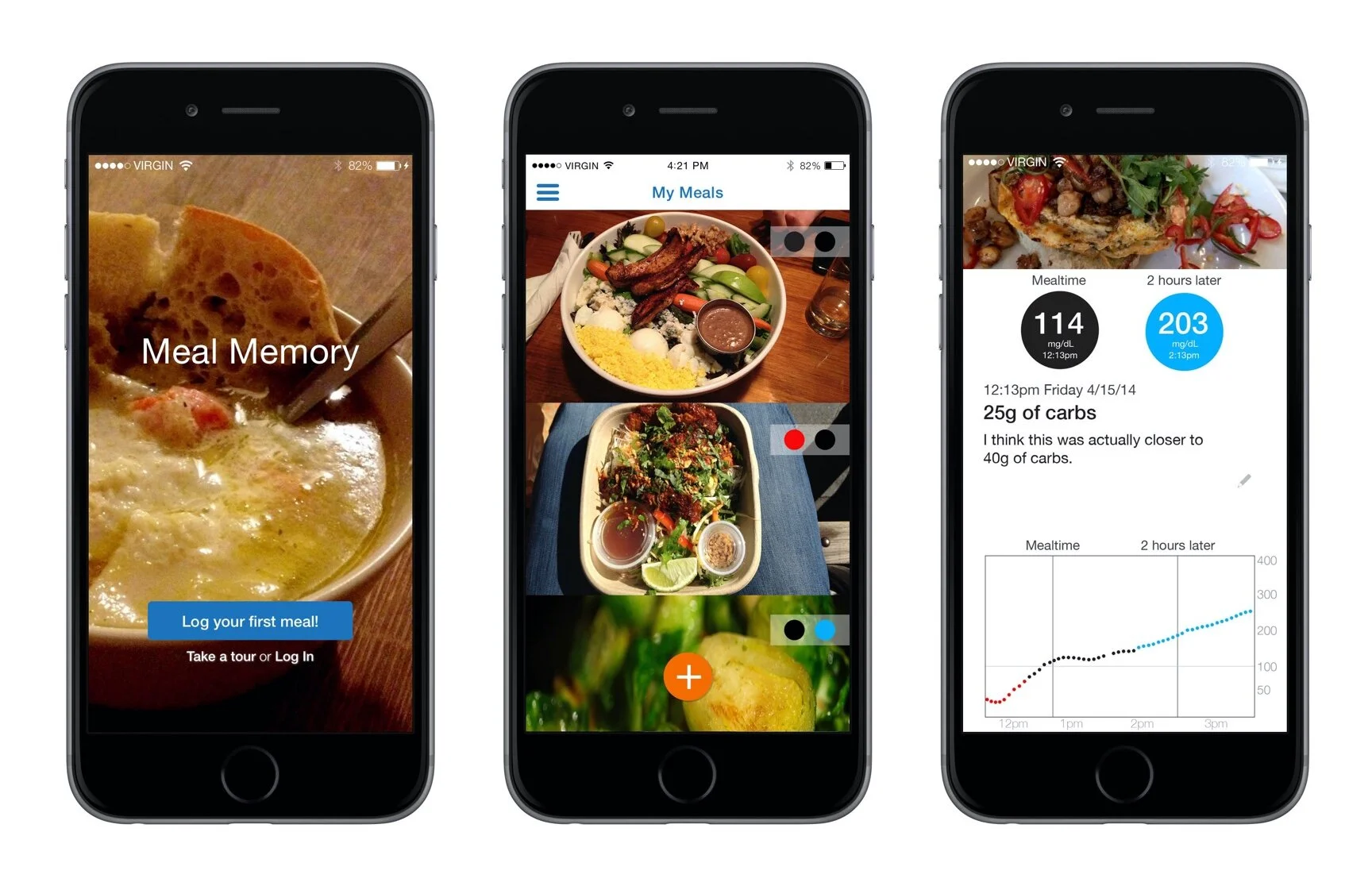
With my goals for the project established, I named the project Meal Memory. By this time, I had a technical cofounder D’Arcy Saum. He worked on the backend while I focused on the design. My ITP classmate and fellow designer Ryan Viglizzo also contributed to early design concepts.
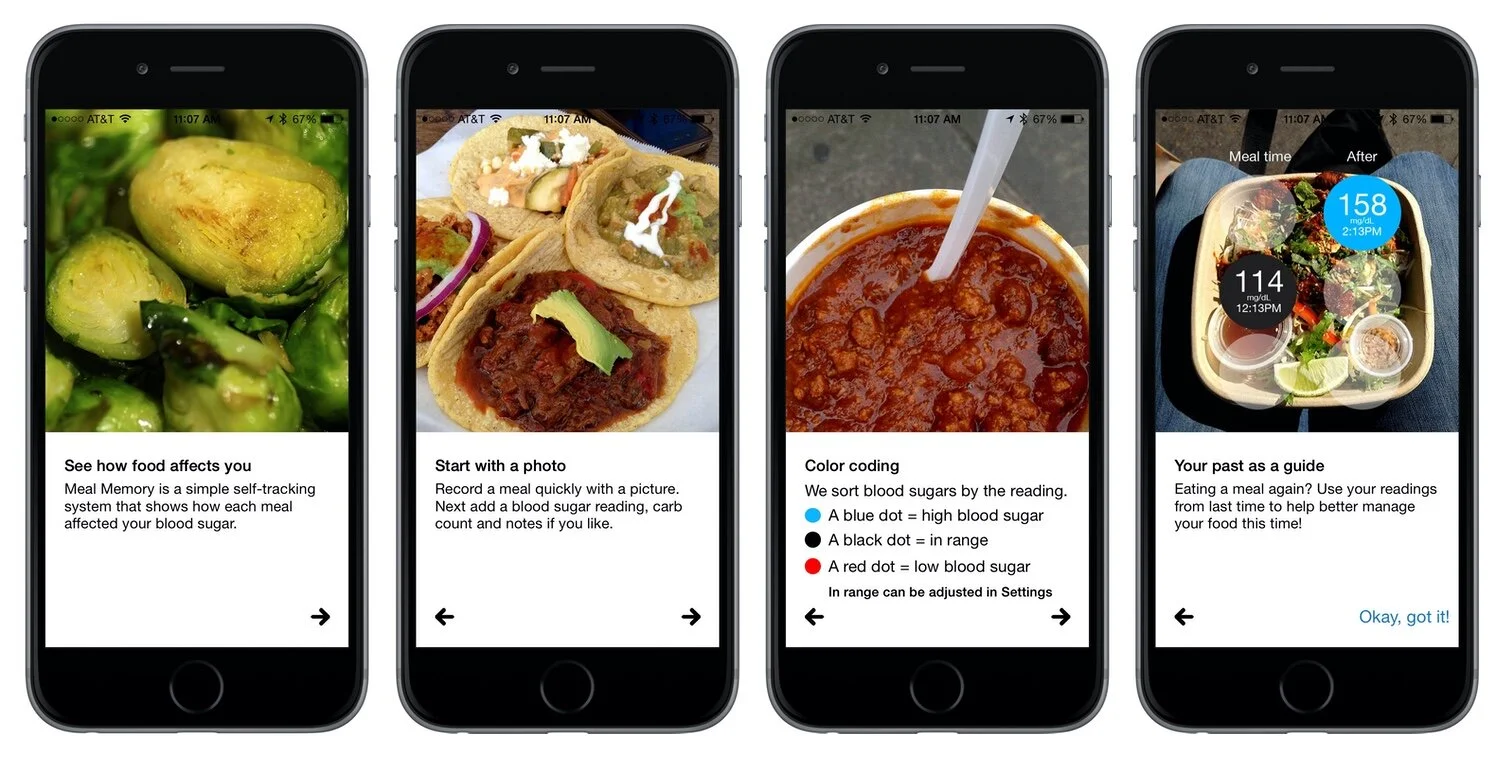
Our small, bootstrapped team aimed to keep the experience as simple as possible. We made account sign up optional and emphasized getting users to log their first meal. Tapping on the + to add a meal entry immediately brought up the camera. It drove the point that photos were central to the experience. A user could also enter an optional carb count.
Another core element of our design was showing glucose readings from before and after eating. At this time, manually entered fingersticks were our only option. Entering a blood glucose reading was required while logging a meal. We then sent a lockscreen notification two hours later asking the users to enter a post-meal glucose.
We also kept the display of data as minimal as possible. The home screen was a chronological photo feed of logged meals. On top of each photo were two color-coded dots. Glucose readings were categorized as either low (red), in range (black), or high (blue). The left dot represented the pre-meal reading, the right the post-meal reading. It gave patients a quick summary of their glucose relative to each meal. Tapping on a photo displayed a detail screen for each entry with additional information, including the exact glucose meal and time/date stamp.
Delivery
Our first version of the Meal Memory mobile app was released for iOS in 2014 with support for manual blood glucose entry. We’d got Meal Memory to market on a shoestring budget. Part of this money came from NYU. During my second year in grad school I’d entered Databetes in the Stern business plan competition. We placed second and won $25k. We were also invited to participate in NYU’s first Summer Launchpad accelerator. This included a small stipend and free office space in their incubator.
Databetes, 2013 NYU Entrepreneur’s Challenge
Dexcom Partnership
Our work on Databetes received a warm welcome from the team at Dexcom, makers of a continuous glucose monitor (CGM). At this time, their G5 system was on the market. They were working on ways to network their data with their Share remote monitoring system. They were also exploring ways to work with Apple.
In 2014, we began working with Dexcom. Apple Health was to be announced soon. Dexcom was preparing to be one of the first diabetes medical devices to allow users to write data to the service. We aligned on a plan to support auto-import of CGM readings directly into Meal Memory via Apple Health. This would benefit users in two ways. First, it removed the need to manually enter glucose readings. Second, it could now display a detailed view of the meal’s impact on glucose with dozens of readings instead of just two.
We released the updated version in time for the 2015 Consumer Electronics Show. Dexcom had a booth at the event and hosted us to showcase the update.
Reactions
Meal Memory struck a chord with fellow patients like Adam Brown, an editor at diaTribe and the diabetes industry consultancy Close Concern. Our app was also frequently mentioned in his book Bright Spots & Landmines. He used it to run his own food and diet experiments to fine tune his control.
Project 2: Nutrition Data Strategy
Joining Dexcom
The success of Meal Memory was one factor in Dexcom’s interest in my work. In 2017, Databetes struck an agreement where I joined Dexcom as a Senior Manager of User Experience Strategy. This was the end of one interesting phase in my career and the start of another. With Databetes, I’d been able to experiment with and prove out several important concepts in patient-centric design. With Dexcom, I became a member of a larger team and have greater opportunities to influence the lives of patients with diabetes.
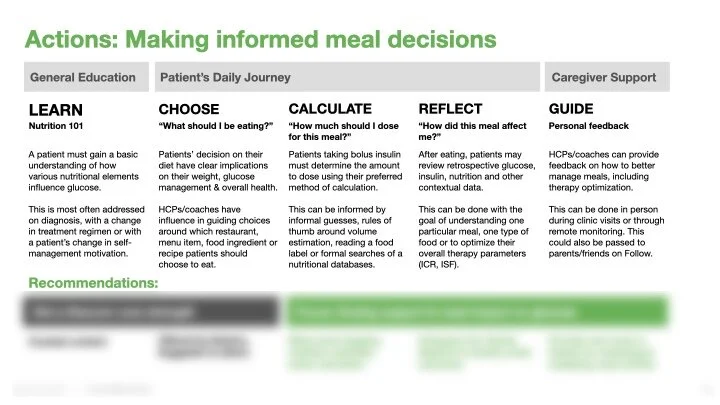
Decision Support
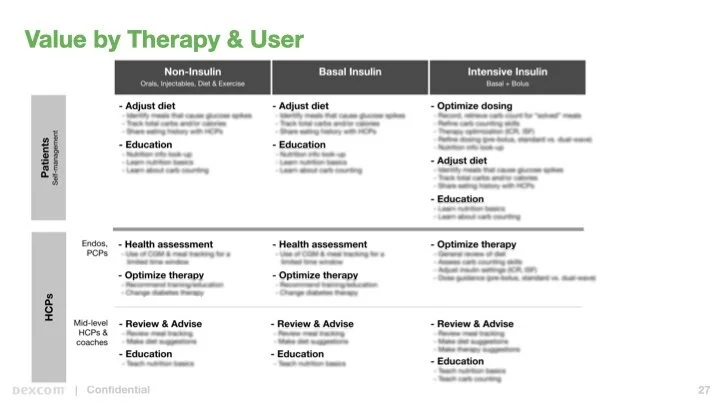
A few months into my new role, I received an assignment to define Dexcom’s Nutrition Data Strategy. This work was a part of Dexcom’s internal Decision Support project. It explored ways of leveraging aggregate data to help patients, healthcare providers, and caregivers with daily treatment decisions.
Competitive Analysis
I looked at a range of apps and services across the diabetes and wellness space. This started with other diabetes management apps like One Drop, mySugr, and Onduo. Also included were diabetes-focused food apps like Calorie Mama and Under My Fork, as well as APIs like Nutrionix and calorie trackers like FatSecret. Noteworthy was Nutrino, a company that would later be acquired by our competitor Medtronic. It provided patients and clinicians with a summary report on logged foods that included a grade on how each meal impacted their glucose. This type of analysis helps patients who might otherwise struggle with turning their logbook into an action plan and list of recommended foods.
Recommendations
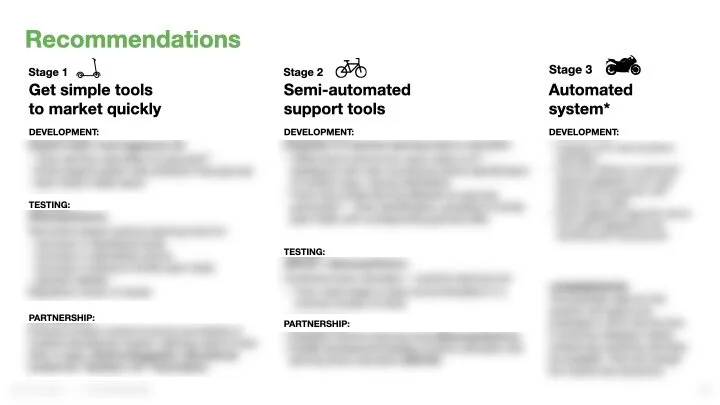
The core of my report was a recommendation on next steps for the organization. I presented a phased plan for providing meal dosing support to our core audience of intensive insulin therapy patients.
By this time, I’d been inside Dexcom long enough to get a better sense of the internal dynamics that affect if, how, and when new features are developed. A 3-phase “crawl, walk, run” approach aimed to get new products to market while also initiating internal projects for testing and evaluation.
My plan started with a Meal Memory-like approach, allowing users to take photos while logging meals and see several hours of pre/post meal glucose readings. Building further, it allowed users to analyze multiple entries of the same meal, supporting patients in “solving” that meal through summary reports. It also recommended integrated nutritional databases, including support for bar code readers.
The final phase looked to explore machine learning tools that recognize food content, correlate it with nutritional databases, and assist patients in meal dosing decisions. We pitched this tool as “Shazam for diabetes,” referencing the app that listens to music and can identify the artist, song, and album. The expectation was that users would use it selectively, most likely for help with challenging meals that seem to occur while eating out. We looked at several vendors of this technology including Bite.ai, makers of the app Bitesnap.
Getting from a photo to a recommended insulin dose is a 4 step process:
Image Recognition: “That looks like ramen.”
Map to a Nutrition Databases: “The average serving of ramen contains 27g of carbs.”
Portion Size Analysis: “This bowl looks like it contains 2 servings.”
Dosing: “Your insulin-to-carb ratio is 1:9, therefore we recommend 6.0u of insulin.”
Tools like these show great promise on auto-completing steps 1 & 2. Yet user input is still required to confirm whether, for example, a glass of soda is either diet or regular. These systems could also be fooled by any dish with ingredients at the bottom of a bowl or otherwise out of sight.
Step 4 is standard math and is the easiest of these to complete. It could be enhanced with personalized analysis that accounts for a person’s eating history (for example, ramen seems to spike your glucose more than rice noodles) or other factors (some patients’ insulin-to-carb ratios are different at different times of day).
This leaves step 3, determining the size of a meal portion. Calculating this with one photo remains a challenge. New platform tools like iOS’ ARkit show promise. Yet these often require viewing an object from multiple angles. This could ultimately complicate the process of logging a meal quickly.
Reaction
My report generated many discussions among the Marketing, Clinical, Regulatory, and R&D teams. The core issues were risk analysis and product vision. Dexcom is a medical device company looking to be a data company. Our revenue is based on sales of hardware and supplies. Our apps are free to all users. How would features like these impact product adoption? How could a tool that assists in dosing decisions be marketed knowing that the technology is still developing?
Several aspects of my report will be integrated into our new G7 system. Others are a work in progress. In the intervening years since presenting this strategy, the market adoption of machine learning tools like Bitesnap has been modest. This is likely to be part a challenge of the technology and part a challenge of user behavior.
As noted at the start of this case study, food and diabetes is a complicated topic. For intensive insulin therapy patients, good glucose control in relation to meals is influenced by food choices, dosing decisions, and the underlying technology. Automated insulin delivery systems, a combination of CGMs, an algorithm, and an insulin pump, are already good and getting better at managing for food. Systems that guide patients with meal dosing decisions will likely return to the spotlight with the adoption of connected insulin pens (Bluetooth devices that will record dosing data). These will address the majority of the insulin dosing market. The hope is that they will allow patients to achieve improved outcomes that rival those of insulin pumps, but at a fraction of the cost. It will be an interesting next step for this promising technology, product design, and new approach to patient support.